The HSE has called on healthcare professionals who are not already working in the public health service to register to be on call during the COVID-19 pandemic.
Apart from the need for extra staff to care for those who will fall ill to COVID-19, there is a recognition that our health service professionals could get sick first and will need to be replaced.
We asked Dr Marie Scully how patients can help protect the health of healthcare professionals who are working on the front line. She said patients are generally abiding by the recommendations not to visit GP practices and her practice has actually seen very few patients in person for the last week. They are, however, dealing with many patients over the telephone. Many have queries in relation to testing for COVID-19.
From 16 March the Irish Government and HSE have taken the view that any patient with respiratory symptoms needs to be referred by their GP for testing so more pressure is expected in the coming weeks.
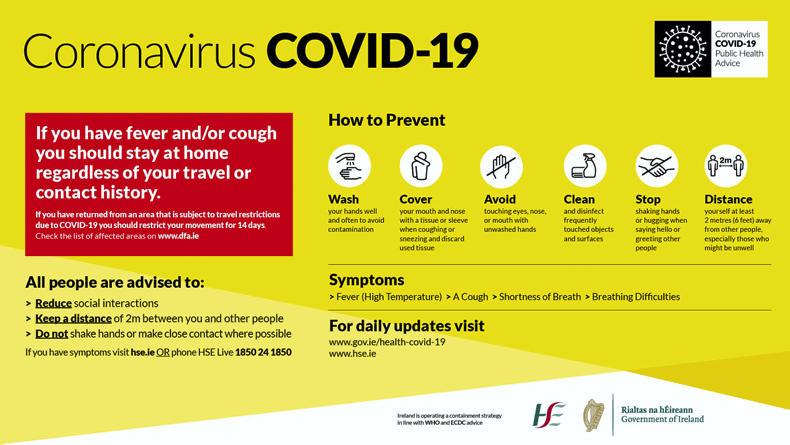
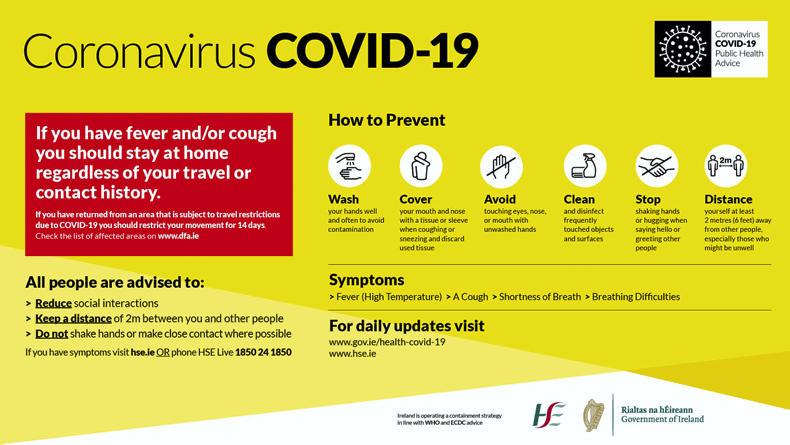
Dr Scully advises that people should look at the hse.ie and hpsc.ie websites as they have a lot of information for the general public.
“To save on the doctor’s time, have a look at the website before ringing the GP’s office as you might get the answer to a general query.”
If you have had a COVID-19 contact, what should you do?
In relation to COVID-19, Dr Scully explains there are two types of contacts which are treated very differently and the first thing that has to be decided is - which are you?
Casual contacts: Brief contact of less than 15 minutes or outside of 2m, such as when you meet someone in the shop or the bank and then later you find out that they tested positive. Many stores have instituted ways eg in queues, to keep people two metres apart. Casual contacts do not need to be self-isolating or tested.Close contacts: If you are within two meters for longer than 15 minutes or a household member of someone who tests positive then you are deemed to be a close contact. If you are an ordinary regular worker who is a close contact but asymptomatic, you will have to self-isolate for 14 days and you have to monitor your symptoms and get tested if you develop any symptoms. There are currently concerns about teenagers. Young people may be less likely to develop severe infection but if they are not social distancing or minding their hand hygiene they may well spread it to their parent or to their grandparent, who might not do so well.
Protocol for suspected COVID-19 patients
“Anybody with respiratory symptoms such as cough, shortness of breath, or a temperature has to stay at home self-isolating and are advised to ring their GP so that they can be referred for testing. In the meantime, they can treat their symptoms with over-the-counter medications such as paracetamol, cough bottles and plenty of rest and fluids.”

Dr Marie Scully.
Dr Scully explains there are two purposes to testing. Firstly, the epidemiology side informs us of how many cases there are. Secondly, as there is a known time frame for this virus, it tells us how long a person needs to self-isolate for and the risk posed to other people in the household.
On testing, if you are COVID-19 negative, you only have to self-isolate for two days after resolution of your symptoms and then you can go back to work.If you are positive for COVID-19, you have to self-isolate for a minimum of 14 days and you have to be fever free for the last five days.“About 80% of people with COVID-19 will have the equivalent of flu-like symptoms that can be managed at home. Of the other 20%, about three-quarters of those will need to go into the hospital because of increasing breathing difficulties but will not necessarily need ICU and ventilation. The other quarter of this 20% [5% of the total] will need ICU and ventilation. These are the people that we are worried about, especially if they have underlying health conditions.
“If you are going to run into complications, and remember this is the minority of people, it is going to be around day seven. If you are getting increasing problems with breathing, shortness of breath and/or chest pains, then you might be one of the unlucky few that end up in hospital. You will be advised to contact your GP again if your symptoms are worsening.”
Advice to protect our frontline staff: your GP
Do not turn up at your GP surgery (or emergency department) without speaking to a doctor first. In most practices, requests for appointments are being triaged and a doctor will call you first.You cannot come into a practice unless the doctor has spoken to you first and has confirmed that you can attend.In the practice, although it may be disconcerting for patients, your doctors and nurses may well be in scrubs, with masks, googles and gloves. If you are on a regular prescription, this is not a problem. But rather than having someone come in to collect it, most practices will fax, e-mail or post scripts to the patient’s pharmacy. Also a new regulation means that a pharmacy can give you a further prescription without one being sent by the doctor. Ring first even if your illness (eg blood pressure, back pain) is completely unrelated to COVID-19.“The main message that I want to get across is that the best way to prevent getting this virus is with hand hygiene and social distancing. This should protect most people and please get your family to do the same,” Dr Scully concluded.
The HSE has called on healthcare professionals who are not already working in the public health service to register to be on call during the COVID-19 pandemic.
Apart from the need for extra staff to care for those who will fall ill to COVID-19, there is a recognition that our health service professionals could get sick first and will need to be replaced.
We asked Dr Marie Scully how patients can help protect the health of healthcare professionals who are working on the front line. She said patients are generally abiding by the recommendations not to visit GP practices and her practice has actually seen very few patients in person for the last week. They are, however, dealing with many patients over the telephone. Many have queries in relation to testing for COVID-19.
From 16 March the Irish Government and HSE have taken the view that any patient with respiratory symptoms needs to be referred by their GP for testing so more pressure is expected in the coming weeks.
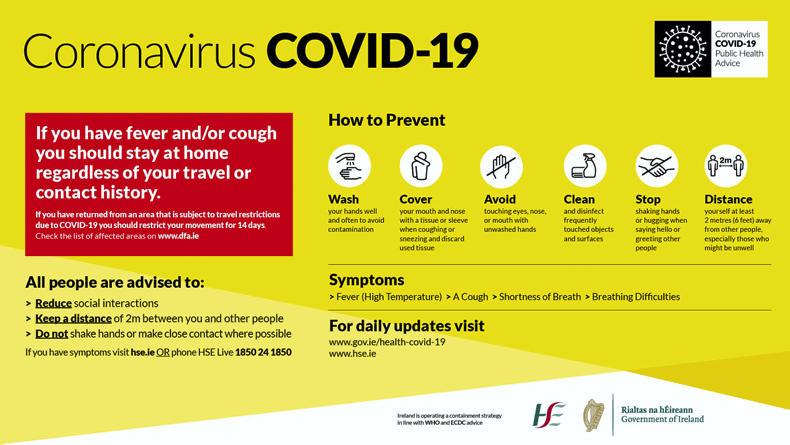
Dr Scully advises that people should look at the hse.ie and hpsc.ie websites as they have a lot of information for the general public.
“To save on the doctor’s time, have a look at the website before ringing the GP’s office as you might get the answer to a general query.”
If you have had a COVID-19 contact, what should you do?
In relation to COVID-19, Dr Scully explains there are two types of contacts which are treated very differently and the first thing that has to be decided is - which are you?
Casual contacts: Brief contact of less than 15 minutes or outside of 2m, such as when you meet someone in the shop or the bank and then later you find out that they tested positive. Many stores have instituted ways eg in queues, to keep people two metres apart. Casual contacts do not need to be self-isolating or tested.Close contacts: If you are within two meters for longer than 15 minutes or a household member of someone who tests positive then you are deemed to be a close contact. If you are an ordinary regular worker who is a close contact but asymptomatic, you will have to self-isolate for 14 days and you have to monitor your symptoms and get tested if you develop any symptoms. There are currently concerns about teenagers. Young people may be less likely to develop severe infection but if they are not social distancing or minding their hand hygiene they may well spread it to their parent or to their grandparent, who might not do so well.
Protocol for suspected COVID-19 patients
“Anybody with respiratory symptoms such as cough, shortness of breath, or a temperature has to stay at home self-isolating and are advised to ring their GP so that they can be referred for testing. In the meantime, they can treat their symptoms with over-the-counter medications such as paracetamol, cough bottles and plenty of rest and fluids.”

Dr Marie Scully.
Dr Scully explains there are two purposes to testing. Firstly, the epidemiology side informs us of how many cases there are. Secondly, as there is a known time frame for this virus, it tells us how long a person needs to self-isolate for and the risk posed to other people in the household.
On testing, if you are COVID-19 negative, you only have to self-isolate for two days after resolution of your symptoms and then you can go back to work.If you are positive for COVID-19, you have to self-isolate for a minimum of 14 days and you have to be fever free for the last five days.“About 80% of people with COVID-19 will have the equivalent of flu-like symptoms that can be managed at home. Of the other 20%, about three-quarters of those will need to go into the hospital because of increasing breathing difficulties but will not necessarily need ICU and ventilation. The other quarter of this 20% [5% of the total] will need ICU and ventilation. These are the people that we are worried about, especially if they have underlying health conditions.
“If you are going to run into complications, and remember this is the minority of people, it is going to be around day seven. If you are getting increasing problems with breathing, shortness of breath and/or chest pains, then you might be one of the unlucky few that end up in hospital. You will be advised to contact your GP again if your symptoms are worsening.”
Advice to protect our frontline staff: your GP
Do not turn up at your GP surgery (or emergency department) without speaking to a doctor first. In most practices, requests for appointments are being triaged and a doctor will call you first.You cannot come into a practice unless the doctor has spoken to you first and has confirmed that you can attend.In the practice, although it may be disconcerting for patients, your doctors and nurses may well be in scrubs, with masks, googles and gloves. If you are on a regular prescription, this is not a problem. But rather than having someone come in to collect it, most practices will fax, e-mail or post scripts to the patient’s pharmacy. Also a new regulation means that a pharmacy can give you a further prescription without one being sent by the doctor. Ring first even if your illness (eg blood pressure, back pain) is completely unrelated to COVID-19.“The main message that I want to get across is that the best way to prevent getting this virus is with hand hygiene and social distancing. This should protect most people and please get your family to do the same,” Dr Scully concluded.










SHARING OPTIONS