Is your home “poison proof”? Are you careful enough about keeping medications and household products out of reach of children?
Over 11,000 worried people, mostly parents, call the National Poisons Information Centre (NPIC) each year seeking advice when something has been consumed that shouldn’t have been consumed.
Fifty per cent of the calls that the National Poisons Information Centre gets every year relate to prescribed and over-the-counter drugs. Sixty-six per cent of enquiries involve children and adolescents with the peak age group for poisoning enquiries being one to four years.
“Paracetamol, ibuprofen and multivitamin preparations are the top three medications involved in child-related medication poisoning queries that we get each year,” Dr Edel Duggan, director of the centre, says.
“About 20% would relate to household products. 4.2% to agricultural products and a few to industrial products as well. Close to 70% of our calls are accidental poisoning related.”
WHAT IS A POISON?
A poison is any substance that can cause harm if it is swallowed, inhaled, injected or absorbed through the skin or eye.
Poisoning can occur with medicines, household products, cosmetics, plants, garden products, farming and industrial chemicals and animals (eg wasp stings).
MOST LIKELY TO HAPPEN IN THE HOME
When it comes to children, most poisoning incidents occur in the child’s home, the home of a grandparent or a childminder or at crèche or school.
Afternoons, weekends and school holidays are the most likely times for this to happen.
“With children, paracetamol is the most common drug involved, probably because of availability of it,” Dr Duggan continues.
“Sometimes, the child just grabs the bottle (of infant pain relief medication) and takes a drink out of it. Sometimes they might have got an extra dose, one parent had given it and then another did, an hour later, not realising that they’d been given it already. The majority of cases happen in the home and it’s mostly children. Toddlers are exploring their environment, picking up things. Most calls relate to children under the under age of five.”
About 40% of the calls to the centre based in Beaumont Hospital, Dublin, come from health professionals – GPs, pharmacists and ambulance or hospital staff.
“There are a few (poisons) we can have antidotes for but we have a huge European database of drug information and we’d be able to tell the health staff what is in the substance and say what management is best. We’d be able to say how the chemicals will affect the person, whether the lungs or the stomach or liver or kidneys will be affected and so on. It’s management guidance for health professionals in that situation.”
Making the call to the National Poisons Information Centre can mean reassurance for parents in minor situations, however.
“While we often advise people to go to their GP or emergency department sometimes people just need reassurance. Being able to talk to our experienced poison information consultants can allay a lot of fear,” she adds.
EXTRA CALLS DURING COVID
COVID-19 lockdowns led to an increase in calls to the National Poisons Information Centre, the director says.
“Hand sanitisers were an issue early on. We had an increase in calls related to children and hand sanitisers in the home, on the first lockdown particularly, when parents were trying to work from home and mind children at the same time.”
FARMING CALLS SMALL BUT SERIOUS
The centre only gets a small percentage of calls related to farm poisoning incidents but they can be quite serious when they do happen, Dr Duggan, who is from a farming family herself, says.
“Calls would relate to pesticides. One of the things we would always recommend is leaving the pesticide in the original container and never putting it into another bottle.
“We had a call a few years ago where a farmer had put a pesticide into a Fanta bottle. He then left it in the car, forgot about it and on a hot day, took a slug out of it.
“It was quite a toxic agent and he ended up in ICU for 10 days, so never transfer products from their original container. Keep all chemicals out of sight and reach of children also so that they don’t get their hands on them. A farmyard isn’t a playground.”
TREATMENT VARIES
Treatment varies with the dosage that has been taken and the concentration of the substance.
“In some cases, there may be an available antidote and in some cases it’s about treating the symptoms. In some cases, there may be medicines that we can get to delay absorption (of the poison). Sometimes we try to get it eliminated (from the body) as quickly as possible. Sometimes we advise on treating the symptoms.”
Treatment depends on the dose, the concentration, the timeframe between when it was taken and when the NPIC was called.
Fifty per cent of the calls that the National Poisons Information Centre gets every year relate to prescribed and over-the-counter drugs.
“The earlier we get the call the greater the chance of preventing the poison from taking effect.”
She points out that inducing vomiting is never recommended as the poison can cause more damage coming up than going down.
In 2020, 7,085 enquiries involved children aged 14 years or under with 52% of those relating to children under the age of four.82.6% of children had no symptoms when the NPIC was contacted.16% had minor or moderate symptoms such as nausea, vomiting, drowsiness or a mild local skin reaction. 10 patients had severe symptoms and there were no fatalities.
– (NPIC 2020 Annual Report)
Products of concern
So, what do we do to make sure that poisoning incidents don’t happen in our homes?
“If you have children or children visit your home regularly go into each room, look around and think about what could potentially be dangerous,” she says.
“The kitchen is particularly important as detergents and dishwasher tablets can be dangerous. Oven cleaners are too.
“They cause a lot of burning in throat and stomach if consumed. Handbags shouldn’t be left lying around either.”
Here is a list of what can be of concern:
Kitchen: detergents, dishwasher tablets, bleach, drain cleaners, oven cleaners, polish, disinfectant, liquid detergent, capsules, white spirit, coins and batteries.Bathroom: medicines, vitamins, iron tablets, bleach, shower cleaner, toilet cleaner, cosmetics, toiletries, shower gel, shampoo, toothpaste and mouthwash.Bedroom: medicines, perfume, aftershave, nail polish remover, essential oils, herbal remedies and false teeth cleaners.Handbags/briefcases:
medicines, coins, hand gel containing alcohol, chewing gum, cigarettes and
e-cigarettes.Shed or garage: petrol, paraffin, car products, insect sprays or powders, rat poison, white spirit, glue, paint and barbecue fluid.Garden: berries, plants (know the names of plants in your garden in case berries are consumed), flowers, mushrooms, slug killer, plant food and weed killer. HANDY LIST to keep your family safe
To keep your family safe from poisoning accidents you should:
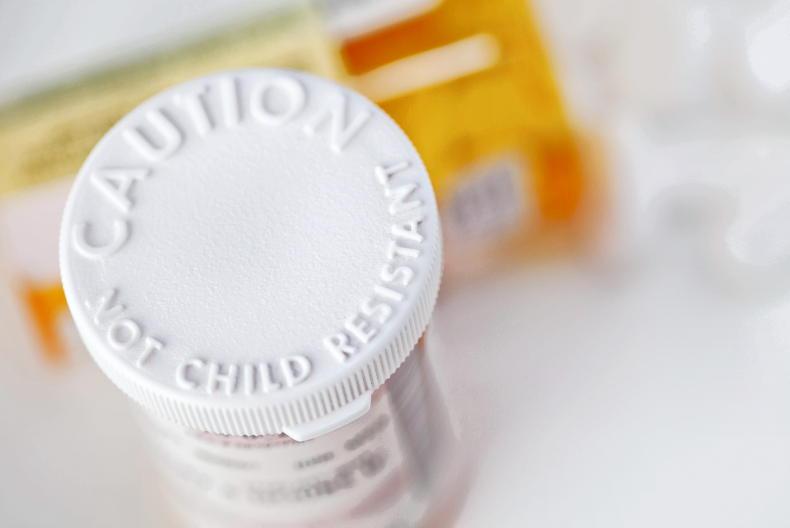
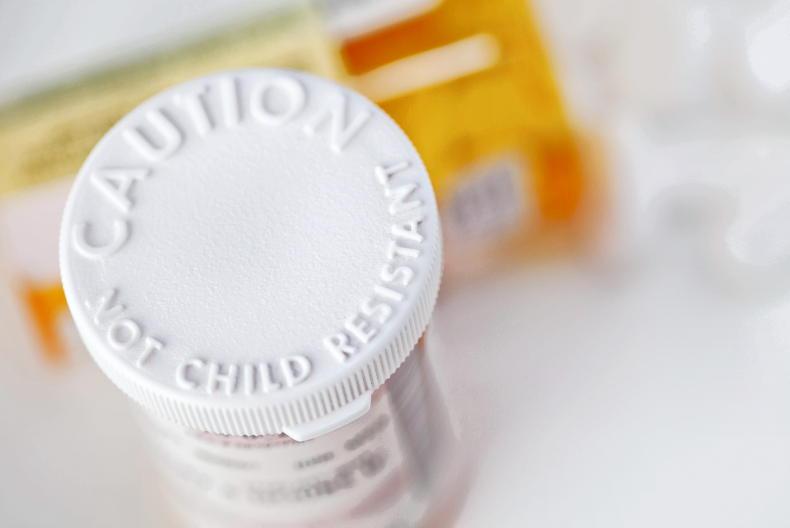
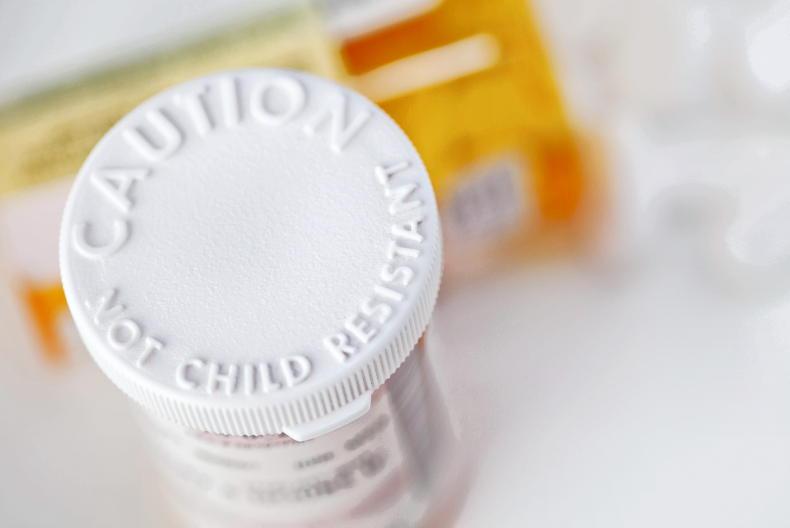
Use containers with child-resistant caps but remember that a child will eventually work it out so keep chemicals and medicines out of reach and out of sight of children as well.Keep all products in their original containers.Use childproof locks on cupboards.Keep handbags that contain medication out of reach. Read medicine labels carefully to avoid mistakes. Ask your GP or pharmacist if you have any questions.Replace all lids on products immediately after use.Ask advice from staff in your garden centre when buying plants.Install carbon monoxide and smoke alarms in your home.What to do if you think your child has been poisoned
What you do in the event of suspected poisoning depends on how serious the situation is, Dr Duggan says.
“If the child is in a serious condition ring an ambulance immediately, of course. Ambulance staff might then ring us for advice but in most cases calls from members of the public come from worried parents who are unsure what to do.”
Advice
Here is the National Poisons Information Centre advice in the event of a child consuming something poisonous/or poisonous if the recommended dosage is exceeded:
Keep calm but act quickly. Take the poison away from the child.Get the child to spit out as much as they can.Look inside the child’s mouth, run your finger around their mouth and take out anything you can. Don’t make your child vomit. This is because the substance could go into the lungs and cause more damage. If the toxic substance has splashed into eyes wash the eyes with tap water for 15 minutes.If a chemical has been in contact with the skin, wash with soap and water. Call the Public Poisons Line - 01 8092166 - 8am to 10pm. Always take the product container with you to the GP or hospital.
Be ready to answer the following
1. What was taken?
2. How much was taken/how much was in the container when you last saw it?
3. What is the child’s age and weight?
4. Does the child have symptoms?
5. Does the child have an existing medical problem?
6. What time did the poisoning occur?
7. Is there information on the container?
8. What is the product used for?
Remember – signs and symptoms may not happen immediately. Always seek advice!
NPIC staff base the advice they give on the worst-case scenario, she states.
“We go on that to cover all bases. We always look for the child’s age and weight to try and calculate whether the child has taken a toxic amount or not.
“As symptoms and signs can be delayed, we would ask parents about the symptoms at that time and give them advice about what to look out for. If certain symptoms develop we would recommend sending them to hospital or GP.
“If a child has other medical conditions he or she may be more vulnerable to a poisoning incident. The information on the container of whatever the child has taken is really important. With our database we can look it up immediately.” CL
Website: www.poisons.ie
Is your home “poison proof”? Are you careful enough about keeping medications and household products out of reach of children?
Over 11,000 worried people, mostly parents, call the National Poisons Information Centre (NPIC) each year seeking advice when something has been consumed that shouldn’t have been consumed.
Fifty per cent of the calls that the National Poisons Information Centre gets every year relate to prescribed and over-the-counter drugs. Sixty-six per cent of enquiries involve children and adolescents with the peak age group for poisoning enquiries being one to four years.
“Paracetamol, ibuprofen and multivitamin preparations are the top three medications involved in child-related medication poisoning queries that we get each year,” Dr Edel Duggan, director of the centre, says.
“About 20% would relate to household products. 4.2% to agricultural products and a few to industrial products as well. Close to 70% of our calls are accidental poisoning related.”
WHAT IS A POISON?
A poison is any substance that can cause harm if it is swallowed, inhaled, injected or absorbed through the skin or eye.
Poisoning can occur with medicines, household products, cosmetics, plants, garden products, farming and industrial chemicals and animals (eg wasp stings).
MOST LIKELY TO HAPPEN IN THE HOME
When it comes to children, most poisoning incidents occur in the child’s home, the home of a grandparent or a childminder or at crèche or school.
Afternoons, weekends and school holidays are the most likely times for this to happen.
“With children, paracetamol is the most common drug involved, probably because of availability of it,” Dr Duggan continues.
“Sometimes, the child just grabs the bottle (of infant pain relief medication) and takes a drink out of it. Sometimes they might have got an extra dose, one parent had given it and then another did, an hour later, not realising that they’d been given it already. The majority of cases happen in the home and it’s mostly children. Toddlers are exploring their environment, picking up things. Most calls relate to children under the under age of five.”
About 40% of the calls to the centre based in Beaumont Hospital, Dublin, come from health professionals – GPs, pharmacists and ambulance or hospital staff.
“There are a few (poisons) we can have antidotes for but we have a huge European database of drug information and we’d be able to tell the health staff what is in the substance and say what management is best. We’d be able to say how the chemicals will affect the person, whether the lungs or the stomach or liver or kidneys will be affected and so on. It’s management guidance for health professionals in that situation.”
Making the call to the National Poisons Information Centre can mean reassurance for parents in minor situations, however.
“While we often advise people to go to their GP or emergency department sometimes people just need reassurance. Being able to talk to our experienced poison information consultants can allay a lot of fear,” she adds.
EXTRA CALLS DURING COVID
COVID-19 lockdowns led to an increase in calls to the National Poisons Information Centre, the director says.
“Hand sanitisers were an issue early on. We had an increase in calls related to children and hand sanitisers in the home, on the first lockdown particularly, when parents were trying to work from home and mind children at the same time.”
FARMING CALLS SMALL BUT SERIOUS
The centre only gets a small percentage of calls related to farm poisoning incidents but they can be quite serious when they do happen, Dr Duggan, who is from a farming family herself, says.
“Calls would relate to pesticides. One of the things we would always recommend is leaving the pesticide in the original container and never putting it into another bottle.
“We had a call a few years ago where a farmer had put a pesticide into a Fanta bottle. He then left it in the car, forgot about it and on a hot day, took a slug out of it.
“It was quite a toxic agent and he ended up in ICU for 10 days, so never transfer products from their original container. Keep all chemicals out of sight and reach of children also so that they don’t get their hands on them. A farmyard isn’t a playground.”
TREATMENT VARIES
Treatment varies with the dosage that has been taken and the concentration of the substance.
“In some cases, there may be an available antidote and in some cases it’s about treating the symptoms. In some cases, there may be medicines that we can get to delay absorption (of the poison). Sometimes we try to get it eliminated (from the body) as quickly as possible. Sometimes we advise on treating the symptoms.”
Treatment depends on the dose, the concentration, the timeframe between when it was taken and when the NPIC was called.
Fifty per cent of the calls that the National Poisons Information Centre gets every year relate to prescribed and over-the-counter drugs.
“The earlier we get the call the greater the chance of preventing the poison from taking effect.”
She points out that inducing vomiting is never recommended as the poison can cause more damage coming up than going down.
In 2020, 7,085 enquiries involved children aged 14 years or under with 52% of those relating to children under the age of four.82.6% of children had no symptoms when the NPIC was contacted.16% had minor or moderate symptoms such as nausea, vomiting, drowsiness or a mild local skin reaction. 10 patients had severe symptoms and there were no fatalities.
– (NPIC 2020 Annual Report)
Products of concern
So, what do we do to make sure that poisoning incidents don’t happen in our homes?
“If you have children or children visit your home regularly go into each room, look around and think about what could potentially be dangerous,” she says.
“The kitchen is particularly important as detergents and dishwasher tablets can be dangerous. Oven cleaners are too.
“They cause a lot of burning in throat and stomach if consumed. Handbags shouldn’t be left lying around either.”
Here is a list of what can be of concern:
Kitchen: detergents, dishwasher tablets, bleach, drain cleaners, oven cleaners, polish, disinfectant, liquid detergent, capsules, white spirit, coins and batteries.Bathroom: medicines, vitamins, iron tablets, bleach, shower cleaner, toilet cleaner, cosmetics, toiletries, shower gel, shampoo, toothpaste and mouthwash.Bedroom: medicines, perfume, aftershave, nail polish remover, essential oils, herbal remedies and false teeth cleaners.Handbags/briefcases:
medicines, coins, hand gel containing alcohol, chewing gum, cigarettes and
e-cigarettes.Shed or garage: petrol, paraffin, car products, insect sprays or powders, rat poison, white spirit, glue, paint and barbecue fluid.Garden: berries, plants (know the names of plants in your garden in case berries are consumed), flowers, mushrooms, slug killer, plant food and weed killer. HANDY LIST to keep your family safe
To keep your family safe from poisoning accidents you should:
Use containers with child-resistant caps but remember that a child will eventually work it out so keep chemicals and medicines out of reach and out of sight of children as well.Keep all products in their original containers.Use childproof locks on cupboards.Keep handbags that contain medication out of reach. Read medicine labels carefully to avoid mistakes. Ask your GP or pharmacist if you have any questions.Replace all lids on products immediately after use.Ask advice from staff in your garden centre when buying plants.Install carbon monoxide and smoke alarms in your home.What to do if you think your child has been poisoned
What you do in the event of suspected poisoning depends on how serious the situation is, Dr Duggan says.
“If the child is in a serious condition ring an ambulance immediately, of course. Ambulance staff might then ring us for advice but in most cases calls from members of the public come from worried parents who are unsure what to do.”
Advice
Here is the National Poisons Information Centre advice in the event of a child consuming something poisonous/or poisonous if the recommended dosage is exceeded:
Keep calm but act quickly. Take the poison away from the child.Get the child to spit out as much as they can.Look inside the child’s mouth, run your finger around their mouth and take out anything you can. Don’t make your child vomit. This is because the substance could go into the lungs and cause more damage. If the toxic substance has splashed into eyes wash the eyes with tap water for 15 minutes.If a chemical has been in contact with the skin, wash with soap and water. Call the Public Poisons Line - 01 8092166 - 8am to 10pm. Always take the product container with you to the GP or hospital.
Be ready to answer the following
1. What was taken?
2. How much was taken/how much was in the container when you last saw it?
3. What is the child’s age and weight?
4. Does the child have symptoms?
5. Does the child have an existing medical problem?
6. What time did the poisoning occur?
7. Is there information on the container?
8. What is the product used for?
Remember – signs and symptoms may not happen immediately. Always seek advice!
NPIC staff base the advice they give on the worst-case scenario, she states.
“We go on that to cover all bases. We always look for the child’s age and weight to try and calculate whether the child has taken a toxic amount or not.
“As symptoms and signs can be delayed, we would ask parents about the symptoms at that time and give them advice about what to look out for. If certain symptoms develop we would recommend sending them to hospital or GP.
“If a child has other medical conditions he or she may be more vulnerable to a poisoning incident. The information on the container of whatever the child has taken is really important. With our database we can look it up immediately.” CL
Website: www.poisons.ie








SHARING OPTIONS