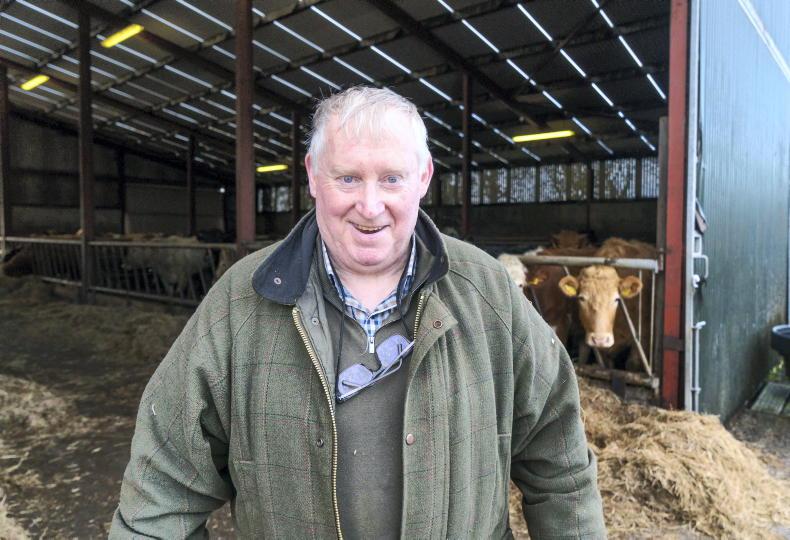
Cystic fibrosis didn’t affect Gordon Ryan from Boyle, Co Roscommon, too much when he was growing up.
“I didn’t feel limited as a child or a teenager at all really,” he says. “That was a bit unusual because a lot of people’s experience with CF is that they would be on antibiotics all through their childhood for lung infections.”
Gordon went on to do an arts degree in legal science and German in UCG after secondary school and decided to do a post-graduate course in law afterwards, at the age of 22. That’s when he became unwell for the first time. In January 2002 he was hospitalised.
“It was bad,” he says. “I was coughing all the time. With CF there’s a lot of thick mucous and your breathing is totally affected. It’s a vicious circle, trying to keep mucous up all the time. You’re totally exposed to lung infections because the mucous is a breeding ground for bacteria. The repeated infections chip away at your lung function so there is a gradual deterioration in your health.”
Gordon’s first lung infection lasted for six weeks and he had another a few months later. Diabetes type two, which often accompanies CF because of the impact the condition has on the digestive system, was also diagnosed.
Illness meant that it took Gordon four years rather than two to finish his post-graduate course.
Accepting that he had cystic fibrosis also took several years, he says.
“It was hard to accept that it wasn’t going to go away because I hadn’t had to deal with it really when I was growing up. Suddenly you’re in your early 20s and you have this foisted upon you. That’s the way it felt.”
There is a rigorous medical routine involved with CF, he adds.
“I had to do half an hour’s physiotherapy every day, mostly involving breathing exercises. Years ago, children used to be thumped on the back (to help clear the mucous in their lungs) but that’s all outdated now,” he says.
“I had to use a nebuliser to loosen the mucous first then use a technique called autogenic drainage. This involves taking breaths at different levels to catch the mucous and gradually move it into your upper airways like an elevator. You start with deep breaths, then deeper ones. It’s an effective technique but it can be hard to learn.”
Failure to clear the mucous would mean a build-up in the lungs and subsequent infection risk.
2002 was a difficult year for Gordon.
“I didn’t deal with the hospitalisation too well initially,” he says.
“When you have CF, there are three of you in the relationship – you and you in terms of what you’re doing – college or work or whatever – and then there’s CF. If you ignore the CF, it becomes like the elephant in the room. It’ll come back on you.
“I was being told that you have to tune in to it and look after it and accept it. That’s the big thing, but that’s difficult because it’s the last thing you want to have to deal with.”
This adjustment is easier for some than others, he adds.
“A nurse told me once that it’s not about getting better, it’s about keeping well. That stuck with me and changed the way I looked at CF. I thought, yeah, this is what it’s about. You have to come to terms with it or it’ll be much harder for you.”
HOSPITAL CONDITIONS
Gordon is very critical of the conditions in hospital for CF patients back then.
“Hospital stays were the absolute pits,” he says. “I was in a general ward, usually with five elderly men who had all sorts of respiratory illnesses, and you’re in there among all that infection.
“CF patients need their own room when they are in hospital for intravenous antibiotics administration, so that they don’t pick up more infection.
“Being in a general ward was like being thrown to the wolves. You’re wide open to infection. It almost defeated the purpose of being in hospital at all.”
The period from 2002-2006/7, when he was in hospital many times, affected him a lot, he says.
“You’d look at hotels and houses going up everywhere but nothing being done for people in hospital. It certainly made me wonder about where people’s priorities lay and how the country was run.”
TRANSPLANT SHOCK
While Gordon was working as a legal assistant in those years, he was forced to give up his job in 2008.
“It got to the point where I couldn’t work. Most of 2008 was spent in hospital and a transplant was first mentioned that summer.”
This came as a shock to Gordon.
“I thought I’d have to face it down the line, but much further down the line, so hearing the consultant mention it was quite frightening.
“I knew it was likely eventually, but the eventually suddenly became very immediate. Every bit of you doesn’t want to make that decision about having the operation, yet you know in your gut that you don’t really have a choice. You know if you leave it too long that you mightn’t get a chance to get one at all.”
EXISTING, NOT LIVING
Gordon had no quality of life for a long time prior to the double lung transplant, he states.
“I was put on oxygen in December 2010. You’re only existing at that stage so from then on I became more at peace with the idea of the transplant.
“That’s important because if you’re not in the right state of mind going into a transplant, you won’t be right coming out of it.”
It had got to the stage where Gordon was in hospital all the time and had a BiPap ventilation mask on 24/7, which did his breathing for him.
“I just took it off to eat. The shocking thing was that it was such a relief to get it back on after eating. It was horrendous really. I knew that I was only going to leave the hospital in one of two ways – with a transplant or in a box. It’s hard to even say that.”
While he was on the UK’s Newcastle list for three years, he decided in June 2013 to put his name on the Mater list. One week later he got the call.
The operation took 13 hours and Gordon was deemed critical for several days afterwards.
“I had bled during the transplant and extra surgeons had to be called down. I got a massive amount of blood, I’m told, nearly 40 litres.”
After four weeks, Gordon was able to get out of bed and was allowed home after 10 weeks.
“That day was fantastic – 30 September. I’d been in hospital since February. Being stuck in hospital was worse than prison. In prison at least you have your health.”
MAJOR TRANSFORMATION
Gordon is now breathing well, thanks to his double lung transplant.
“The big thing is that I’m able to do things now – plan things. I hadn’t been able to do that for years. I’ve been to Wales and Spain – it was so great to be able to turn up at the airport and just head off.”
Since having the transplant, Gordon feels psychologically lighter, he says.
“CF is a physical illness but it has a psychological impact as well. Now I feel lighter in so many ways.”
Gordon is now doing a radio production course and is signing up for a Masters in journalism next September. He is on a lot of anti-rejection medication but says it is a small price to pay.
“You have to see the difference in people before and after a transplant to realise it. They are so vibrant and healthy afterwards.”
ETERNAL GRATITUDE
Gordon thinks of his donor and donor family every day.
“I know it was a hard decision for that family to make. I know that one person being a donor can save maybe five lives with all the different organs. That’s such a marvellous thing. I’ll be eternally grateful for my transplant. Saying it’s the gift of life sounds like a cliché but it’s true. You have to have gone through it to fully understand how wonderful it is.
“It was the incredible support of my family and friends which helped me through those difficult times over the many years before and after the transplant. I was blessed to have that.”
*It’s not really known why Ireland has a higher rate of CF patients in the world but island countries tend to have higher numbers because the CF gene is more likely to be reproduced. One in 19 Irish people carry the CF gene.
National awareness
Cystic Fibrosis Ireland’s 65 Roses National Awareness Week runs from 20-26 April. The event is named after the way in which children are first taught to pronounce the words cystic fibrosis. You can organise your own 65 event or contribute if you see street collectors selling pins during that awareness week. You can also make a donation of €2 by texting “65ROSES” to 50300.
While there has been an improvement in CF services in recent years, there is much more to do, according to GAA commentator Joe Brolly: “We need to invest more in post-transplant support, in treatments, facilities and research,” he says. “We also need to address issues of access to education, travel, housing and employment for people with CF.”
For more information, LoCall 1890-311-211 or visit www.cfireland.ie. To request a donor card now, see www.organdonation.ie or freetext DONOR to 50050 or LoCall 1890-543-639.








SHARING OPTIONS