Skin cells multiplying too rapidly – that sums up the inflammatory skin condition, psoriasis.
The average person’s skin renews every 28-30 days or so, the skin of a person who has psoriasis renews every two to three days. Therefore, the person ends up with thick, silvery skin scales (layers of skin) and itchy, dry, red patches that can be painful. Scalp, elbows and knees are often affected first. There is no cure for it, unfortunately, but treatments can help control it.
While it is not contagious and never infectious, it can have a debilitating effect on the person who has it, however.
“It’s an impact on sufferers that is often underestimated or unrecognised,” says Dublin-based dermatologist, Professor Brian Kirby. “Psoriasis should never be characterised as a ‘bit of a rash’. It remains a highly stigmatised condition, often because the general population doesn’t know much about it. Many people with it suffer in silence. It’s important for anyone who has it to know that resources and support are available.”
Almost one in four people with the condition suffer from depression at some point in their lives, he adds.
People with psoriasis are also more prone to suffering from high blood pressure and 30% will develop psoriatic arthritis as a result of having moderate to severe psoriasis, statistics say.
Recently, Professor Kirby spoke during the Irish Skin Foundation #SaySomething campaign, to increase awareness about psoriasis.
The Irish Skin Foundation was founded in 2011, to inform and support patients with all forms of skin diseases, such as psoriasis, eczema, rosacea and acne.
The campaign launched a diagnostic questionnaire and a short online film on the foundation’s website www.irishskinfoundation.ie
Its aim is to encourage patients to speak more openly to their doctor about all their symptoms – something that doesn’t always happen, as many people hide the real impact it has on them, according to the experts.
Psoriasis –
several types
There are several types of psoriasis:
• Plaque psoriasis – most common.• Guttate – red, scaly dots, like drops of water, on the body.• Nummular – round plaques the size of a coin.• Pustular – affects hands and feet.• Erythrodermic psoriasis – most severe kind, plaque and pustules.• Flexural psoriasis – affects skin folds and creases.Triggers
Triggers can be different for different people, but can include the following:
• Streptococcal infections.• Cold weather.• Stress. • Medication.• Skin injury, eg cuts or scrapes.• Alcohol, smoking and obesity.• Infection, eg sore throat.Tips for living with psoriasis
• Exercise regularly and get as much rest as you need to maintain health and reduce stress.• Avoid excess alcohol – it makes psoriasis worse.• Eat a healthy, balanced diet – obesity also worsens psoriasis. • Don’t smoke – again, it worsens the condition.• Use relaxation techniques, meditation and exercise to reduce stress.• Keep a diary to pinpoint situations, places or events that trigger your stress. Understanding your triggers can help you manage your psoriasis better.The websites below offer free CBT and mindfulness-based tools to help with stress and anxiety.
• www.papaa.org/self-help/etips • www.beaumont.ie Treatments
No treatment can cure psoriasis, but some treatments may control or clear it. Treatment depends on the severity and location of your psoriasis.
Treatments can be divided into three main types:
1. Topical treatments (eg creams applied to the skin, on prescription).2. Ultraviolet light therapy.3. Sytemic treatments – oral or injected drugs for severe cases. The #SaySomething initiative is supported by Abbvie.
Avoid flare-ups
1. Don’t scrub your skin. 2. Don’t bathe in hot water. 3. Keep your skin moist. 4. Wear cotton. 5. Cut your nails. Moisturising makes a difference
Caroline Irwin from Kilkenny has psoriasis, and is the former chairperson of the Psoriasis Association of Ireland. She is now a board member of the newly set up Irish Skin Foundation.
She had some sound advice for those with the condition.
“Moisturising properly is the key to getting the most out of prescription creams,” she says. “Rubbing them onto scaly patches is no good – you have to shower or bathe using emollients to soften the scales first then put the prescription creams on after that. That way you get more relief.
“There are lots of different combinations of creams available now. People say to me: ‘Ah I went to the doctor years ago and got cream and it was no good’.
“Doctors now give more detailed instructions about how to use the creams. I was doing it wrong for 30 years. Some people have never even asked their GP to refer them to a dermatologist either, that’s something they should consider.”
Explaining psoriasis to children and teenagers
There are some good books available through the website to help you do this. For example,
Ted, a Little Story About Me (illustrated) and Aoife – Living with Psoriasis (for teenagers who have psoriasis). Let’s Talk About Psoriasis (a guide for parents, teachers, sports coaches and friends of older children with the condition) is also a good option.
Emollient focus
There are many emollients available in pharmacies for showering, bathing and moisturising. Remember, products that suit some people won’t suit others. Expert advice says to always try a patch test first, particularly when using an emollient with a topical steroid. Emollients on the market include Aveeno, E45, Elave, Eucerin, Lipikar Ap, Oilatum and Vaseline Intensive Rescue. Remember AQUEOUS CREAM is NOT an emollient. It is a soap substitute and recent research has shown that it can make skin conditions worse if left on the skin. Discuss the emollient options with your GP, dermatologist, nurse or pharmacist.
Living with psoriasis
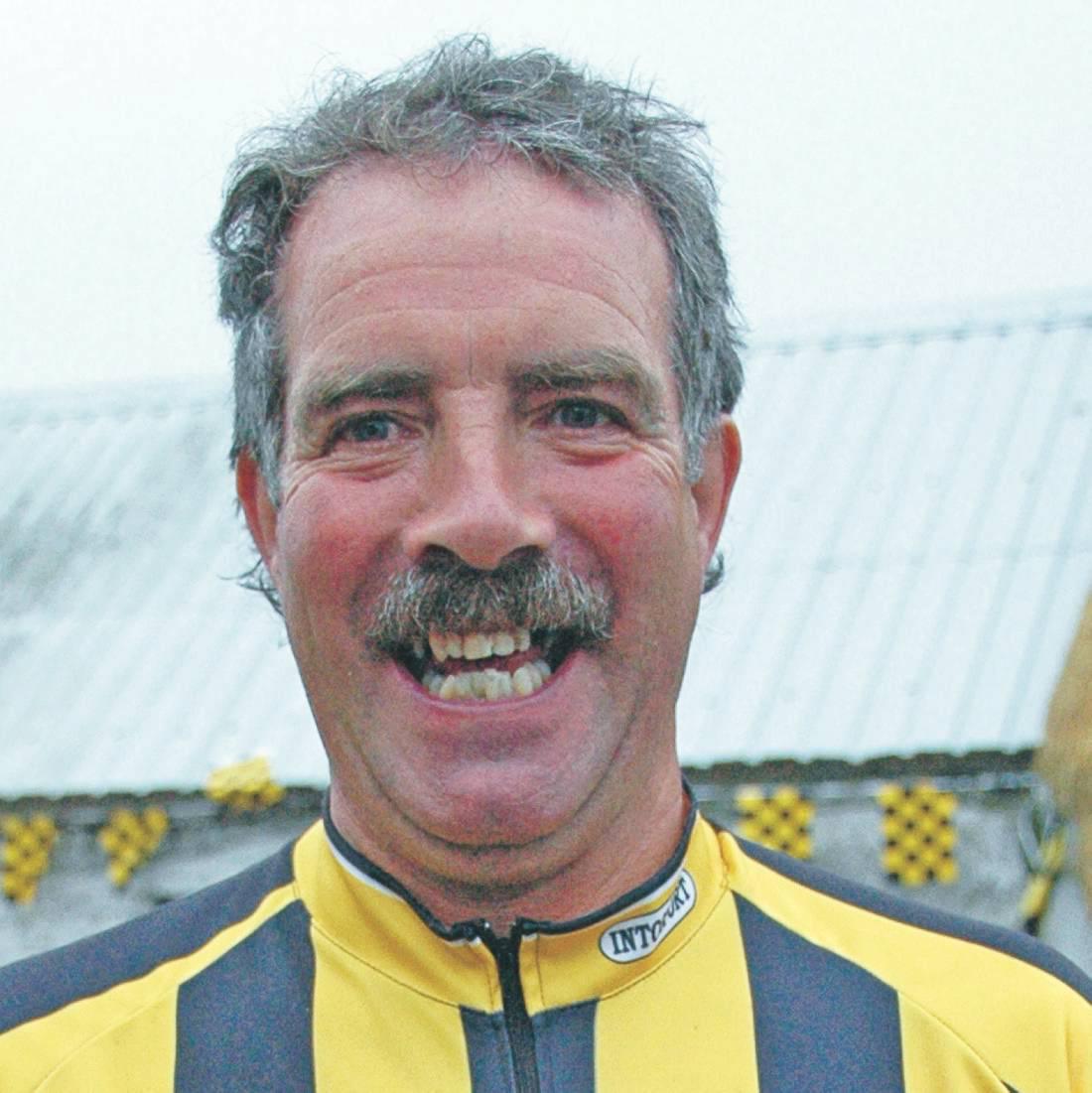
Michael Brennan from Ballyfoyle, Co Kilkenny, has had psoriasis for the past 30 years. While it is a condition that he’d prefer to wake up without, it doesn’t stop him doing anything he wants to do, he says.
Michael advises anyone newly diagnosed with it to not get too hung up on it.
“It started in a small way with me,” the landscape gardener told Irish Country Living, “with blotches on my arms and then on my legs. I didn’t rush to the doctor because I’d seen my father with a few patches on his legs before he died and helped him put cream on them over the years, but we didn’t really have a name for what the condition was.
“I think I said it to the doctor in passing one day when I went to see him about a chest infection. He looked at it not as a life-threatening condition, but as something that you just have to treat and live with, and that’s the way I look at it. While at times you’d like to wake up in the morning without it, you have to get on with your life.”
Having psoriasis did make him feel a bit self-conscious early on, however.
“I was playing badminton at the time and I’d always wear tracksuits, never shorts, because of it. It would affect your confidence a bit all right. Also, swimming for me was a no. I won’t say chlorine in the water affected it, but it did give more of a redness to it. You would be self-conscious in a togs too, thinking people would be looking.”
Michael used topical steroid creams to treat it in the early years.
“While they did ease it, they never totally cleared it,” he says, “and doctors don’t want you to stay on those types of creams too long. At the moment I use E45 cream (an emollient) every morning, evening and after a shower. That stops the flakiness and eases the itch for me. Other people find other moisturisers suit them, it’s very individual, and it may take a while to find the one that suits you best. Even though there’s a blanket name for it – psoriasis – there are several different forms of it, so every person is affected differently. I have the more blotchy (plaque) type.”
Michael finds that it flares up occasionally, but not regularly and not for any particular reason.
“It’s something in the body that causes it to get a little more aggressive and flare up a bit more now and then,” he says. “I don’t get that stressed, generally, but I find that in winter it could be a bit worse because of the friction from wearing heavier clothes.”
Michael believes that awareness of the condition has improved among the public.
“You see more people with it and people are more open now about a lot of things,” he says.
“If someone says to me: ‘Did you hurt yourself?’, or ‘Have you a rash?’, I say: ‘No, it’s psoriasis’, just like that. It’s no big deal anymore.”
While keeping the plaque areas moist lessens the itch and flakiness, there is the inconvenience of skin shedding.
“You leave a trail of flakes on the carpet, unfortunately,” he says.
Michael hasn’t chosen to take oral or injected biologic medication for his psoriasis.
“I didn’t look at it as serious enough an issue to require that, for me anyway, but there’s people with it worse than mine, who do use them. Initially, I suppose I was looking for a cure, but now I know about it and just get on with it. It’s very individual how you handle it.”
What would he say to anyone who is newly diagnosed with psoriasis?
“Try to manage it as best you can and use whatever treatment is suited to it, but don’t be too hung up on it.
“Life goes on and it’s not a life-threatening condition and there are creams and cosmetics to cover over, if you want. The other thing to remember is that you’re not alone. It’s quite widespread, so a lot of people have it and there’s a lot of help and information out there now.”
Skin cells multiplying too rapidly – that sums up the inflammatory skin condition, psoriasis.
The average person’s skin renews every 28-30 days or so, the skin of a person who has psoriasis renews every two to three days. Therefore, the person ends up with thick, silvery skin scales (layers of skin) and itchy, dry, red patches that can be painful. Scalp, elbows and knees are often affected first. There is no cure for it, unfortunately, but treatments can help control it.
While it is not contagious and never infectious, it can have a debilitating effect on the person who has it, however.
“It’s an impact on sufferers that is often underestimated or unrecognised,” says Dublin-based dermatologist, Professor Brian Kirby. “Psoriasis should never be characterised as a ‘bit of a rash’. It remains a highly stigmatised condition, often because the general population doesn’t know much about it. Many people with it suffer in silence. It’s important for anyone who has it to know that resources and support are available.”
Almost one in four people with the condition suffer from depression at some point in their lives, he adds.
People with psoriasis are also more prone to suffering from high blood pressure and 30% will develop psoriatic arthritis as a result of having moderate to severe psoriasis, statistics say.
Recently, Professor Kirby spoke during the Irish Skin Foundation #SaySomething campaign, to increase awareness about psoriasis.
The Irish Skin Foundation was founded in 2011, to inform and support patients with all forms of skin diseases, such as psoriasis, eczema, rosacea and acne.
The campaign launched a diagnostic questionnaire and a short online film on the foundation’s website www.irishskinfoundation.ie
Its aim is to encourage patients to speak more openly to their doctor about all their symptoms – something that doesn’t always happen, as many people hide the real impact it has on them, according to the experts.
Psoriasis –
several types
There are several types of psoriasis:
• Plaque psoriasis – most common.• Guttate – red, scaly dots, like drops of water, on the body.• Nummular – round plaques the size of a coin.• Pustular – affects hands and feet.• Erythrodermic psoriasis – most severe kind, plaque and pustules.• Flexural psoriasis – affects skin folds and creases.Triggers
Triggers can be different for different people, but can include the following:
• Streptococcal infections.• Cold weather.• Stress. • Medication.• Skin injury, eg cuts or scrapes.• Alcohol, smoking and obesity.• Infection, eg sore throat.Tips for living with psoriasis
• Exercise regularly and get as much rest as you need to maintain health and reduce stress.• Avoid excess alcohol – it makes psoriasis worse.• Eat a healthy, balanced diet – obesity also worsens psoriasis. • Don’t smoke – again, it worsens the condition.• Use relaxation techniques, meditation and exercise to reduce stress.• Keep a diary to pinpoint situations, places or events that trigger your stress. Understanding your triggers can help you manage your psoriasis better.The websites below offer free CBT and mindfulness-based tools to help with stress and anxiety.
• www.papaa.org/self-help/etips • www.beaumont.ie Treatments
No treatment can cure psoriasis, but some treatments may control or clear it. Treatment depends on the severity and location of your psoriasis.
Treatments can be divided into three main types:
1. Topical treatments (eg creams applied to the skin, on prescription).2. Ultraviolet light therapy.3. Sytemic treatments – oral or injected drugs for severe cases. The #SaySomething initiative is supported by Abbvie.
Avoid flare-ups
1. Don’t scrub your skin. 2. Don’t bathe in hot water. 3. Keep your skin moist. 4. Wear cotton. 5. Cut your nails. Moisturising makes a difference
Caroline Irwin from Kilkenny has psoriasis, and is the former chairperson of the Psoriasis Association of Ireland. She is now a board member of the newly set up Irish Skin Foundation.
She had some sound advice for those with the condition.
“Moisturising properly is the key to getting the most out of prescription creams,” she says. “Rubbing them onto scaly patches is no good – you have to shower or bathe using emollients to soften the scales first then put the prescription creams on after that. That way you get more relief.
“There are lots of different combinations of creams available now. People say to me: ‘Ah I went to the doctor years ago and got cream and it was no good’.
“Doctors now give more detailed instructions about how to use the creams. I was doing it wrong for 30 years. Some people have never even asked their GP to refer them to a dermatologist either, that’s something they should consider.”
Explaining psoriasis to children and teenagers
There are some good books available through the website to help you do this. For example,
Ted, a Little Story About Me (illustrated) and Aoife – Living with Psoriasis (for teenagers who have psoriasis). Let’s Talk About Psoriasis (a guide for parents, teachers, sports coaches and friends of older children with the condition) is also a good option.
Emollient focus
There are many emollients available in pharmacies for showering, bathing and moisturising. Remember, products that suit some people won’t suit others. Expert advice says to always try a patch test first, particularly when using an emollient with a topical steroid. Emollients on the market include Aveeno, E45, Elave, Eucerin, Lipikar Ap, Oilatum and Vaseline Intensive Rescue. Remember AQUEOUS CREAM is NOT an emollient. It is a soap substitute and recent research has shown that it can make skin conditions worse if left on the skin. Discuss the emollient options with your GP, dermatologist, nurse or pharmacist.
Living with psoriasis
Michael Brennan from Ballyfoyle, Co Kilkenny, has had psoriasis for the past 30 years. While it is a condition that he’d prefer to wake up without, it doesn’t stop him doing anything he wants to do, he says.
Michael advises anyone newly diagnosed with it to not get too hung up on it.
“It started in a small way with me,” the landscape gardener told Irish Country Living, “with blotches on my arms and then on my legs. I didn’t rush to the doctor because I’d seen my father with a few patches on his legs before he died and helped him put cream on them over the years, but we didn’t really have a name for what the condition was.
“I think I said it to the doctor in passing one day when I went to see him about a chest infection. He looked at it not as a life-threatening condition, but as something that you just have to treat and live with, and that’s the way I look at it. While at times you’d like to wake up in the morning without it, you have to get on with your life.”
Having psoriasis did make him feel a bit self-conscious early on, however.
“I was playing badminton at the time and I’d always wear tracksuits, never shorts, because of it. It would affect your confidence a bit all right. Also, swimming for me was a no. I won’t say chlorine in the water affected it, but it did give more of a redness to it. You would be self-conscious in a togs too, thinking people would be looking.”
Michael used topical steroid creams to treat it in the early years.
“While they did ease it, they never totally cleared it,” he says, “and doctors don’t want you to stay on those types of creams too long. At the moment I use E45 cream (an emollient) every morning, evening and after a shower. That stops the flakiness and eases the itch for me. Other people find other moisturisers suit them, it’s very individual, and it may take a while to find the one that suits you best. Even though there’s a blanket name for it – psoriasis – there are several different forms of it, so every person is affected differently. I have the more blotchy (plaque) type.”
Michael finds that it flares up occasionally, but not regularly and not for any particular reason.
“It’s something in the body that causes it to get a little more aggressive and flare up a bit more now and then,” he says. “I don’t get that stressed, generally, but I find that in winter it could be a bit worse because of the friction from wearing heavier clothes.”
Michael believes that awareness of the condition has improved among the public.
“You see more people with it and people are more open now about a lot of things,” he says.
“If someone says to me: ‘Did you hurt yourself?’, or ‘Have you a rash?’, I say: ‘No, it’s psoriasis’, just like that. It’s no big deal anymore.”
While keeping the plaque areas moist lessens the itch and flakiness, there is the inconvenience of skin shedding.
“You leave a trail of flakes on the carpet, unfortunately,” he says.
Michael hasn’t chosen to take oral or injected biologic medication for his psoriasis.
“I didn’t look at it as serious enough an issue to require that, for me anyway, but there’s people with it worse than mine, who do use them. Initially, I suppose I was looking for a cure, but now I know about it and just get on with it. It’s very individual how you handle it.”
What would he say to anyone who is newly diagnosed with psoriasis?
“Try to manage it as best you can and use whatever treatment is suited to it, but don’t be too hung up on it.
“Life goes on and it’s not a life-threatening condition and there are creams and cosmetics to cover over, if you want. The other thing to remember is that you’re not alone. It’s quite widespread, so a lot of people have it and there’s a lot of help and information out there now.”










SHARING OPTIONS