Will we be toasting the success of the Sláintecare programme in 10 years’ time? That’s the €6bn euro question.
While the name is inspiring – ‘sláintecare’ meaning ‘good health care’ – will it mean that by 2028 we don’t have to put our hands in our pockets every time we see a doctor? Will it put an end to long waiting lists and trolleys on corridors, as well as those who can afford private medical insurance being seen quicker?
Maybe we shouldn’t hold our breath – patients may have to be patient and visions take a while to realise, but at least there appears to be a good road map for reform now.
While it’s tempting to say that we’ve heard all the promises before, this is the first cross-party plan to improve the health service, so there seems to be the political consensus to make it happen.
The promises are huge – free GP and public hospital care for all, scans and x-rays available quickly at GP surgeries rather than in hospitals, cuts to the prescription charge, more nurses, home helps, physios.
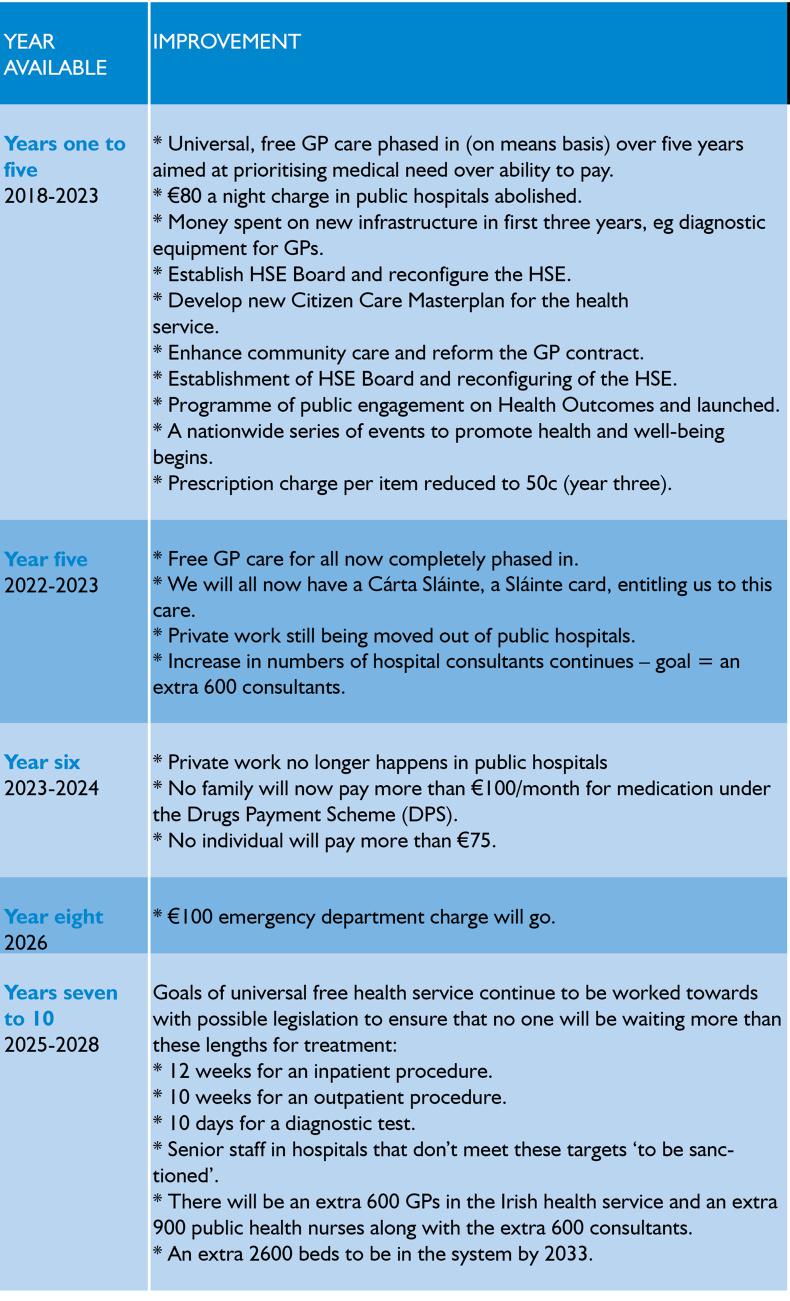
Overall, the table gives a bird’s eye view of what the all-party plan entails and the timeframe for completion. Please note that at the time of writing the crucial decision that is meant to be one of the cornerstones of Sláintecare – taking private care out of public hospitals – is still being analysed.
Costs
This is where the fogginess comes in. While there is a definite figure of €3bn to be spent on infrastructure early on, the Minister for Health says that for diagnostic equipment for GPs and more staff – like physios, home helps, social workers and speech and language therapists – the cost of Sláintecare will be dependent on “very serious” contractual negotiations that will occur over time with GPs and consultants.
GP and consultant contracts are always tough to negotiate and a new GP contract is already long-awaited, so should we hold our breath?
There was also much criticism about the lack of costings for the programme – €6bn is the figure to be spent over the 10 years, including capital expenditure and transitional funding, with an initial €3bn investment.
A figure of €455m was mentioned as the cost of phasing-in universal free GP care, but doctors’ representative organisations say this is a gross underestimation.
Employing an extra 600 hospital consultants is going to cost about €119m, for example. That’s each consultant getting €198,333. The single-tier system will be funded through a combination of general taxation revenues and earmarking of some taxes, levies or charges into a single National Health Fund, with promises that it will be ‘ringfenced’.

What is promised?
So what are the promises? The Sláintecare report was published last year with assurances that if the programme was implemented it would get rid of the two-tier system in the health service.
Also, think healthcare shifting out of hospitals and more into primary care, community settings. Think patients getting scans and test results locally, within days. Think patients with chronic disease being better looked after locally, thereby eliminating emergency department fire brigade visits.
Think no more private patients passing public patients out in queues for treatment because there are no queues.
Think some hospitals being built that will just do elective (planned) surgery.
What could stop this working?
Public hospital managers won’t be happy with €650m/year dropping out of their income from private health insurers. Who is going to make up that deficit? The taxpayer? The goal is laudable though – to free up beds for more public health care and bring down public waiting times, but the disentanglement of public and private care could meet many obstacles and an impact analysis has yet to be done.What if tax hikes are necessary to bring in Sláintecare, as the Health Insurance Authority predicts? Will TDs have the backbone to still support the programme in this situation?Those with cheaper private health insurance policies could have to pay up to €300 more for higher-end private hospital plans, the VHI says. That’s because private care in public hospitals has been a feature of cheaper policies. The Health Insurance Authority (HIA) estimates that Sláintecare will mean that private health insurance cover in this country will drop from 45% of the population to 30% over 15 years. In the UK, where the National Health Service exists, only 10% of the population has such cover. Private hospitals could close.At least one of the current private sector insurers could be forced out of the market.GP and consultant contract negotiations will be complex and lengthy.The National Treatment Purchase Fund will need more investment to tackle waiting lists.Where will the extra 600 consultants, 600 GPs and 900 practice nurses be found? Will those now working abroad have enough faith in Sláintecare to want to come back to work in Ireland?Reaction
Hospital consultants say that the figure of €2.68 bn over 10 years is a major underestimation. The Irish Cancer Society says that the Sláintecare Implementation Strategy is an “important step on the road to universal healthcare in Ireland, but highlighted the absence of costings”. The Royal College of Physicians says it “sets out a clear roadmap for much needed reform” and “if properly resourced and implemented” is an opportunity to build a patient-centred health system. The National Association of General Practioners (NAGP) is seriously disappointed over the absence of costings. It says there is nothing new in it. “Without proper funding for GP-led primary care and Sláintecare, these assurances are meaningless.”An Taoiseach Leo Varadkar
“The publication of the Sláintecare Implementation Strategy … provides the framework for a significant programme of change and improvement to achieve the long-term vision as set out in the Sláintecare report.”
Minister Simon Harris
“This is the vision. If you are working in the health service today…and you are working bloody hard and are wondering if there is light at the end of the tunnel: this is that. This is how we are going to get there. We are not going to get there overnight. We are going to work with you, we are going to engage with you.
“The implementation strategy being published today outlines a sustainable programme of reform for the coming years.
“It is firmly rooted in the vision and underpinning principles of the Sláintecare report. The reform programme reaches right across all health services, and will be complex. These changes won’t happen overnight, and it is essential to get the sequencing of reform right to minimise interference with ongoing service delivery and to put in place the necessary enablers and building blocks for reform, including infrastructure and supports for the health workforce.”
Dr Tom Keane, chair of the Sláintecare Advisory Council
“Strong leadership, clear governance and effective engagement of stakeholders across the health sector will be essential to successful reform, as will a long-term vision for health policy that remains constant from government to government – that is what Sláintecare represents.”
Ms Laura Magahy
She led the Temple Bar urban renewal project, and the proposed project to relocate Temple Street children’s hospital to the Mater hospital site will see her take up position as director of the Sláintecare programme in September.
Ms Magahy will be tasked with refining the Implementation Strategy into a more detailed action plan within three months of taking office.
The Sláintecare Implementation Strategy is available at www.gov.ie/Sláintecare
Will we be toasting the success of the Sláintecare programme in 10 years’ time? That’s the €6bn euro question.
While the name is inspiring – ‘sláintecare’ meaning ‘good health care’ – will it mean that by 2028 we don’t have to put our hands in our pockets every time we see a doctor? Will it put an end to long waiting lists and trolleys on corridors, as well as those who can afford private medical insurance being seen quicker?
Maybe we shouldn’t hold our breath – patients may have to be patient and visions take a while to realise, but at least there appears to be a good road map for reform now.
While it’s tempting to say that we’ve heard all the promises before, this is the first cross-party plan to improve the health service, so there seems to be the political consensus to make it happen.
The promises are huge – free GP and public hospital care for all, scans and x-rays available quickly at GP surgeries rather than in hospitals, cuts to the prescription charge, more nurses, home helps, physios.
Overall, the table gives a bird’s eye view of what the all-party plan entails and the timeframe for completion. Please note that at the time of writing the crucial decision that is meant to be one of the cornerstones of Sláintecare – taking private care out of public hospitals – is still being analysed.
Costs
This is where the fogginess comes in. While there is a definite figure of €3bn to be spent on infrastructure early on, the Minister for Health says that for diagnostic equipment for GPs and more staff – like physios, home helps, social workers and speech and language therapists – the cost of Sláintecare will be dependent on “very serious” contractual negotiations that will occur over time with GPs and consultants.
GP and consultant contracts are always tough to negotiate and a new GP contract is already long-awaited, so should we hold our breath?
There was also much criticism about the lack of costings for the programme – €6bn is the figure to be spent over the 10 years, including capital expenditure and transitional funding, with an initial €3bn investment.
A figure of €455m was mentioned as the cost of phasing-in universal free GP care, but doctors’ representative organisations say this is a gross underestimation.
Employing an extra 600 hospital consultants is going to cost about €119m, for example. That’s each consultant getting €198,333. The single-tier system will be funded through a combination of general taxation revenues and earmarking of some taxes, levies or charges into a single National Health Fund, with promises that it will be ‘ringfenced’.

What is promised?
So what are the promises? The Sláintecare report was published last year with assurances that if the programme was implemented it would get rid of the two-tier system in the health service.
Also, think healthcare shifting out of hospitals and more into primary care, community settings. Think patients getting scans and test results locally, within days. Think patients with chronic disease being better looked after locally, thereby eliminating emergency department fire brigade visits.
Think no more private patients passing public patients out in queues for treatment because there are no queues.
Think some hospitals being built that will just do elective (planned) surgery.
What could stop this working?
Public hospital managers won’t be happy with €650m/year dropping out of their income from private health insurers. Who is going to make up that deficit? The taxpayer? The goal is laudable though – to free up beds for more public health care and bring down public waiting times, but the disentanglement of public and private care could meet many obstacles and an impact analysis has yet to be done.What if tax hikes are necessary to bring in Sláintecare, as the Health Insurance Authority predicts? Will TDs have the backbone to still support the programme in this situation?Those with cheaper private health insurance policies could have to pay up to €300 more for higher-end private hospital plans, the VHI says. That’s because private care in public hospitals has been a feature of cheaper policies. The Health Insurance Authority (HIA) estimates that Sláintecare will mean that private health insurance cover in this country will drop from 45% of the population to 30% over 15 years. In the UK, where the National Health Service exists, only 10% of the population has such cover. Private hospitals could close.At least one of the current private sector insurers could be forced out of the market.GP and consultant contract negotiations will be complex and lengthy.The National Treatment Purchase Fund will need more investment to tackle waiting lists.Where will the extra 600 consultants, 600 GPs and 900 practice nurses be found? Will those now working abroad have enough faith in Sláintecare to want to come back to work in Ireland?Reaction
Hospital consultants say that the figure of €2.68 bn over 10 years is a major underestimation. The Irish Cancer Society says that the Sláintecare Implementation Strategy is an “important step on the road to universal healthcare in Ireland, but highlighted the absence of costings”. The Royal College of Physicians says it “sets out a clear roadmap for much needed reform” and “if properly resourced and implemented” is an opportunity to build a patient-centred health system. The National Association of General Practioners (NAGP) is seriously disappointed over the absence of costings. It says there is nothing new in it. “Without proper funding for GP-led primary care and Sláintecare, these assurances are meaningless.”An Taoiseach Leo Varadkar
“The publication of the Sláintecare Implementation Strategy … provides the framework for a significant programme of change and improvement to achieve the long-term vision as set out in the Sláintecare report.”
Minister Simon Harris
“This is the vision. If you are working in the health service today…and you are working bloody hard and are wondering if there is light at the end of the tunnel: this is that. This is how we are going to get there. We are not going to get there overnight. We are going to work with you, we are going to engage with you.
“The implementation strategy being published today outlines a sustainable programme of reform for the coming years.
“It is firmly rooted in the vision and underpinning principles of the Sláintecare report. The reform programme reaches right across all health services, and will be complex. These changes won’t happen overnight, and it is essential to get the sequencing of reform right to minimise interference with ongoing service delivery and to put in place the necessary enablers and building blocks for reform, including infrastructure and supports for the health workforce.”
Dr Tom Keane, chair of the Sláintecare Advisory Council
“Strong leadership, clear governance and effective engagement of stakeholders across the health sector will be essential to successful reform, as will a long-term vision for health policy that remains constant from government to government – that is what Sláintecare represents.”
Ms Laura Magahy
She led the Temple Bar urban renewal project, and the proposed project to relocate Temple Street children’s hospital to the Mater hospital site will see her take up position as director of the Sláintecare programme in September.
Ms Magahy will be tasked with refining the Implementation Strategy into a more detailed action plan within three months of taking office.
The Sláintecare Implementation Strategy is available at www.gov.ie/Sláintecare









SHARING OPTIONS